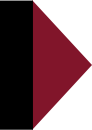
- Blood transfusion, a life-saving procedure somewhat taken for granted today, has a long history of trial and error.
- From transfusion of animal blood to using milk instead of blood to alleviate adverse blood transfusion reactions, the history of blood transfusion has been one marked by human suffering.
- At the beginning of the 20th century blood typing to cross-check compatibility between donor and recipient was discovered, but it was not until the 1930s that the Rh factor was recognized as the most common cause of blood transfusion reactions.
Blood transfusion is a common life-saving tool today in the practice of medicine, but it wasn’t long ago that it was a hit-or-miss procedure with as good or better a chance of killing the patient instead of saving a life.
Blame It On the Four Humors
In centuries past, blood was considered one of the four “humors” that made up living matter: Blood, phlegm, yellow bile, and black bile. From ancient Greece to the Age of Renaissance, these four elements were said not only to work together to order the nutrition, growth and metabolism of the body but also to dictate specific personality traits.
Blood (air, hot and wet), as the essence of vitality, was said to embody joy, optimism and well-being; phlegm (water, cold and wet) was associated with passivity, lethargy and emotional sensitivity; yellow bile (fire, hot and dry) was thought to provoke the emotions of excitability, such as passion, anger and courage; and black bile (earth, cold and dry) was charged with promoting caution, pessimism and melancholy.1
Animal “Studies”
The first blood transfusions were done between animals, with one often-repeated story involving draining the blood of one dog into another, while the recipient’s own blood was drained out its other side. In that 1666 experiment, the first dog died from blood loss, but the other recovered and was expected to do fine with the donor blood.2
According to the diary of one who was there, this “did give occasion to many pretty wishes, as of the blood of a Quaker to be let into an Archbishop and such like; but may if it takes be of might us to man’s health for the mending of bad blood by borrowing from a better body.”3 This sentiment reflects the ongoing belief in the four humors, assuming that desired personality traits might be transfused along with blood. True to this tenet, the earliest attempts at transfusing blood into a human were not for blood loss but rather to treat psychological disorders.
During the late 1600s, for example, scientists reported successful transfusion of sheep’s blood into humans.4 The sheep’s blood was intended to impart the docility of the sheep nature into a patient with an agitated or “overheated” personality. A relatively infamous case involved a 15-year-old boy—previously treated with leeches to suck out his bad blood—treated by Jean-Baptiste Denys, personal physician to King Louis XIV. That boy reportedly lived, though the assumption today is that the reason he survived was that the amount of sheep’s blood used (about 12 ounces) was too small to cause a fatal reaction.
Dr. Denys’s subsequent trials were not so successful. Some patients died and the wife of one sued him for murder, effectively ending both his career and the practice of transfusing animal blood into humans.5 The history of blood transfusion disappears there and doesn’t show up again for almost 200 years.
The Seeds of Modern Medicine
The earliest successful transfusions between human patients are credited to James Blundell in 1880, when he saved the life of a woman with postpartum hemorrhage by transfusing blood from her husband.6 This initial triumph was reportedly followed up with several other human blood transfusions for physical ailments involving blood loss, such as stomach tumors, half of which were successful and half “not,” presumably meaning that the patient died.
Given what we now know about blood compatibility, it sounds about right that half of the patients might have survived, by chance receiving donor blood they could tolerate because it was a compatible blood type. However, since medical practice had surpassed biological understanding, the high rate of failures drove the scientists away from human-to-human blood transfusion and toward using more “neutral” fluids to replace lost blood. Milk was one of the most popular substances substituted for blood, and goat, cow and human milk were commonly used up until 1880, particularly in the United States.7
Adverse reactions and poor outcomes were common and, by 1884, saline infusion had replaced milk as a routinely used blood substitute.8
Not All Human Blood Is the Same
Finally in 1900—about the time it was discovered that mosquito control could significantly reduce the incidence of yellow fever and malaria9—a breakthrough f came that would change the future of blood transfusion: Austrian physician Karl Landsteiner discovered the first three types of blood, for the first time showing that not all human blood is the same. He designated his findings as types “A,” “B,” and “C” (later changed to “O”). His colleagues later added “AB” as the fourth blood type, completing the OBO system we still abide by today.10
It took until 1907, when Emil von Behring was experimenting with mixing diphtheria toxin and antitoxin to develop a vaccine that would protect but not cause the disease11—before it was discovered that cross-matching blood types between blood donors and recipients of blood could lead to better health outcomes.12
Prospects for blood recipients were much improved after it was recognized that certain blood types were incompatible with others, but there was still a pretty good chance patients suffering devastating adverse reactions from human to human blood transfusions.
We Are Still Learning
It was not until 1939 that Karl Landsteiner (the same man who had originally recognized the different blood types) characterized the Rh blood system,13 which involves a complex interplay among more than 49 antigens on the surface of red blood cells. Among those many antigens, it is the D, C, c, E, and e that have been most clearly characterized. The D antigen has gotten the most attention because it is most likely to cause compatibility problems between a mother and her unborn baby. When someone is classified as Rh- it generally refers to the D antigen.14 15
The Rh blood system represents yet another example of just how different peoples can be and demonstrates once again emphasizes once again that a “one size fits all” approach in medicine is both unscientific and dangerous because it fails to acknowledge and respect genetic and biological differences between individuals.
References:
1 Osborn DK. Agents of Metabolism. Greek Medicine.net 2015.
2 Blackwell Science Ltd. Historical Review: The History of Blood Transfusion. British Journal of Haematology Dec. 24, 2001.
3 See Footnote 1.
4 History of Blood Transfusions. American Red Cross.
5 June 15, 1667:First Human Blood Transfusion; With Sheep’s Blood! History and Headlines June 15, 2017.
6 Rowlinson, M. On the First Medical Blood Transfusion Between Human Subjects, 1818. BRANCH: Britain, Representation and Nineteenth-Century History. Ed. Dino Franco Felluga. Extension of Romanticism and Victorianism on the Net. Web. September 2017.
7 See Footnote 4.
8 Highlights of Transfusion Medicine History. AABB: Advancing Transfusion and Cellular Therapies Worldwide 2017.
9 The History of Vaccines. The College of Physicians of Philadelphia 2017.
10 See Footnote 8.
11 See Footnote 9.
12 See Footnote 4.
13 See Footnote 4.
14 O’Neil D. Rh Blood Types. Anthro.palomar.edu 2013.
15 NIH. Blood Groups and Red Cell Antigens [Internet]. National Center for Biotechnology Information. Apr. 18, 2016.










3 Responses
Thank you for this walk through medical history – this is an excellent parallel to the “primitive” practice of modern-day conventional medicine’s only “preventative” medical procedure. My reason for posting is to say that the validity/credibility of some point of view, especially if the topic is controversial, can be negatively affected if there are typo’s or other grammatical oversights within the text, as there are in this. I think it worthwhile, no, really important, to have several persons carefully scrutinize articles such as this for any errors. Just one oversight can be enough to dismiss an otherwise extremely important and authoritative message. Thank you.
Thank you for that history. I had no idea blood transfusions went back that far in time. I have a question and have not known whom to ask. I’ve been wondering if blood transfusions from people who’ve had diseases like measles could be given to those with a bad case of the disease to help them fight it off. Would the antibodies in the blood of measles survivors provide enough passive immunity to help those with weak immune systems?
Yes, a “one size fits all” approach does not work for vaccines either. But that is only one facet of the problem.
Unlike with blood transfusions, we have a government trying to determine how to treat every single person.
Central planning, in all its many guises, never works. We should not have government bureaucrats trying to dictate our health care needs in the first place, whether there solution is one-size, 2-size, or 50-size.