During the peak of the COVID-19 pandemic, several countries in Africa were praised for controlling the pandemic by implementing traditional public health strategies to contain the spread of the SARS-CoV-2 virus, despite having underdeveloped and fragile public heath systems. With a population of more than one billion people, the African continent appears to have been far less affected by the pandemic than the Americas, Europe and Asia in terms of poor health outcomes and mortality.1
According to a study conducted by Partnership for Evidence-based Response to COVID-19 (PERC), a public-private partnership that supports evidence-based measures to reduce the impact of COVID on African Union member states:
The case-fatality ratio (CFR) for COVID-19 in Africa is lower than the global CFR, suggesting the outcomes have been less severe among African populations.3
There has been speculation that data collection related to deaths in many African countries is not accurate. However, only 34.6 percent of countries globally have complete death registration data in the Civil Registration and Vital Statistics (CRVS), while most African countries at least have a data collection system in place, and there is no evidence that COVID mortality data is less accurately reported in Africa than in other regions. The only African country that has not been reporting COVID cases and deaths in the past three years is Tanzania.3
A Younger Age Demographic in Africa
There are several factors believed to have contributed to fewer death cases attributed to COVID cases in Africa,4 including the age of the population in most African countries, which is likely to have played a role in containing the spread of SARS-CoV-2.5 Most COVID-related deaths occurred in people aged 65 or older. The median age in North and South America, Europe, and Asia ranges from 32 to 42.5 years, while the median age in Sub-Saharan Africa is 18 years old.6
“We have [in Africa] about 3 percent of the population aged over 65 years, said Dr. Matshidiso Moeti, the World Health Organization’s (WHO) regional director for Africa.7
Low Rate of Pre-Existing Conditions Such as Chronic Diseases in Africa
The medical literature has shown that patients with pre-existing conditions such as diabetes, chronic respiratory diseases, obesity, and hypertension have an increased risk of moderate to severe complications from SARS-CoV-2 infection. These chronic poor health conditions are considerably less prevalent in low income and lower middle-income countries when compared to higher income countries, which may provide a possible explanation for why the COVID burden is relatively lower in Africa. African countries have a low prevalence of non-communicable chronic diseases compared to 88 percent in the United States and 74 percent in Brazil.8
Does the Absence of Long-Term Care Facilities in Africa Reduce COVID Transmission?
Most elderly people in Africa do not live in long-term care facilities. These facilities tend to increase the risk of transmission of infectious diseases. In most African countries, care of elderly family members is mostly left to the family, thus reducing the risk of infection transmission. In the beginning of the pandemic, about 81 percent of deaths from COVID in Canada occurred in long-term care facilities.9
Does the Hygiene Hypothesis Play A Role in Lower COVID Mortality in Africa?
There has been some concern that regions which use ultra-hygienic public health practices, such as the overuse of hand sanitizer and other disinfection interventions favored in many developed countries, may reduce microbial exposure and create a disadvantage for populations to effectively meet the immunological challenge of new viruses, such as SARS-CoV-2. Researchers agree that this hypothesis is plausible and can be observed in the differences observed in the burden of chronic diseases between richer and poorer countries.10
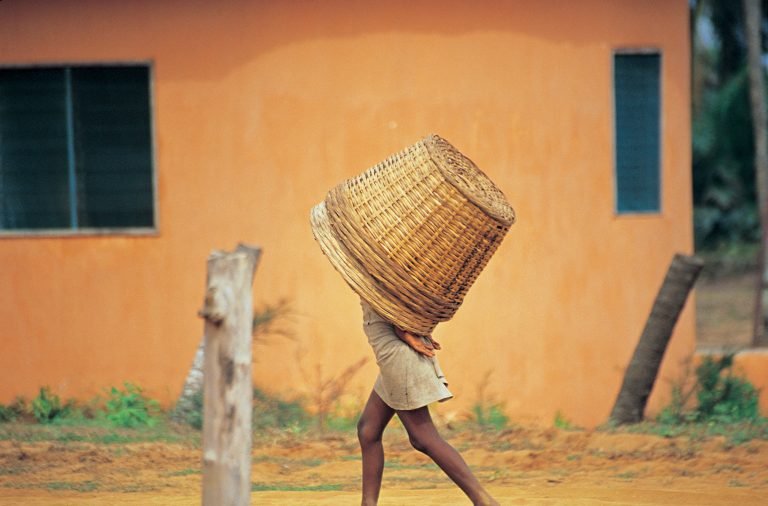
Outdoor Lifestyles with More Exposure to Sunlight in African Nations
Typical African lifestyles involve working in agriculture outdoors from sunrise to sunset, with shelters used mostly for sleeping. Research shows people living in rural areas spend far more time outdoors than people living in urban areas. Articles published in the medical literature suggest that exposure to sun increases vitamin D production and reduces the severity of COVID symptoms, which may explain why Africans engaged in year-round outdoor living with direct exposure to UV sunlight in mostly warm and tropical climates are experiencing fewer COVID complications and deaths.11
Africa Has Lowest Covid Vaccination Rates
As of July 2022, only 24.4 percent of the population in Africa had received at least one dose of a COVID shot in comparison with the global average of 69 percent.12 Only three African countries, Liberia, Mauritius and Seychelles have 70 percent of their population vaccinated.13 Studies conducted by Africa CDC and various researchers have shown a lack of trust in COVID shots across communities in Africa.14
The WHO said even though less than a quarter of all Africans have been vaccinated, the number of COVID shots given in Africa has dropped by more than 50 percent over the last three months.15
If you would like to receive an e-mail notice of the most recent articles published in The Vaccine Reaction each week, click here.
Click here to view References:1 Soy A. Coronavirus in Africa: Five reasons why Covid-19 has been less deadly than elsewhere. UNICEF Oct. 9, 2020.
2 Ibid.
3 Wamai R. What Could Explain the Lower COVID-19 Burden in Africa despite Considerable Circulation of the SARS-CoV-2 Virus? International Journal of Environmental and Public Health August 2021; 18(16): 8638.
4 Ezeh A, Silverman M, Stranges S. Why has Covid-19 had less of an impact in Africa? Quartz Aug. 23, 2021.
5 Soy A. Coronavirus in Africa: Five reasons why Covid-19 has been less deadly than elsewhere. UNICEF Oct. 9, 2020.
6 Ezeh A, Silverman M, Stranges S. Why has Covid-19 had less of an impact in Africa? Quartz Aug. 23, 2021.
7 Soy A. Coronavirus in Africa: Five reasons why Covid-19 has been less deadly than elsewhere. UNICEF Oct. 9, 2020.
8 Wamai R. What Could Explain the Lower COVID-19 Burden in Africa despite Considerable Circulation of the SARS-CoV-2 Virus? International Journal of Environmental and Public Health Augusut 2021; 18(16): 8638.
9 Ezeh A, Silverman M, Stranges S. Why has Covid-19 had less of an impact in Africa? Quartz Aug. 23, 2021.
10 Wamai R. What Could Explain the Lower COVID-19 Burden in Africa despite Considerable Circulation of the SARS-CoV-2 Virus? International Journal of Environmental and Public Health August 2021; 18(16): 8638.
11 Wamai R. What Could Explain the Lower COVID-19 Burden in Africa despite Considerable Circulation of the SARS-CoV-2 Virus? International Journal of Environmental and Public Health August 2021; 18(16): 8638.
12 Chen et al. A data-driven approach to addressing COVID-19 vaccine uptake in Africa. McKinsey Aug. 2, 2022.
13 Larson K. COVID vaccination rates have dropped 50% in Africa, WHO says. Los Angeles Times Oct. 20, 2022.
14 Chen et al. A data-driven approach to addressing COVID-19 vaccine uptake in Africa. McKinsey Aug. 2, 2022.
15 Larson K. COVID vaccination rates have dropped 50% in Africa, WHO says. Los Angeles Times Oct. 20, 2022.











5 Responses
You missed one important point. Many places in Africa fight malaria with regular doses of Ivermectic or hydroxychloroquine. This may have acted as a prophylactic against Covid.
Did they study and/or account for the greater use of Ivermectin in these populations?
Excellent article.
They got some good excuses.
But they are only excuses.
We have the death rate from COVID per age group. and yes most death were over 75 years old, but we can estimate what Africa ? death rate is compare to US by age group.
If US want to reduce COVID ☠️ , then US would have investigated all country, and found out what worked.
How about not paying for medical treatment if they die. That would give the hospital reason to cure COVID.
Or we could shame the hospital by report their success rate. Who would choose a hospital that killed their customers ?
How could we possibly shame them. The health “profession” has shown us over the last few years that they have no shame.